Has the WHO lost its way regarding alcohol?


A particularly balanced, thoughtful take on the current wine-and-health debate, from David Morrison, who has kindly allowed us to republish this article from his data-driven wine blog, The Wine Gourd.
As I am sure that most wine-related people have noticed, the World Health Organization (WHO) has recently (since early 2023) taken a very negative formal stance with regard to alcohol consumption (No level of alcohol consumption is safe for our health). This is quite a change of tune from its previous writings, which reported some protective associations of low to moderate alcohol consumption.
Other wine commenters have been doubtful about discussing either the science or the medicine behind the WHO (eg What the debate about wine and health gets wrong; Yes, we are all doomed to die. But wine won’t do us in). Well, my professional background is in biological science, and so I will do so. It seems to me that the WHO’s current official stance is, in at least some ways, absurd. I will discuss this here, focusing specifically on wine as the source of alcohol. It is quite a long post, but please bear with me.
The WHO’s change of tune has actually been coming gradually over the past decade. However, this topic has come to the fore recently, at least partly because the US federal government is currently revising its dietary guidelines (Alcohol policies in U.S. states, 1999–2018), and it has been made quite clear that these are likely to recommend a major reduction in alcohol use (Biden’s alcohol czar warns Americans could soon be told to limit themselves to just two beers per week under strict new booze guidelines). The wine industry has now woken up (The Barbarians are at the gate).
Well it seems to me that the WHO is attacking wine for no good science reason. Having read their documentation (cited above), their principal claim is that there is no acceptable proof of the health safety of any amount of alcohol. Therefore, they conclude that alcohol must be avoided.
This conclusion is arrant nonsense. Even if their premise is correct (no evidence), then their conclusion (avoid) does not necessarily follow. If there is almost no scientific ‘proof’ one way or the other, as far as health is concerned, then given their own claims, the best that the WHO can do is be neutral on the matter.1
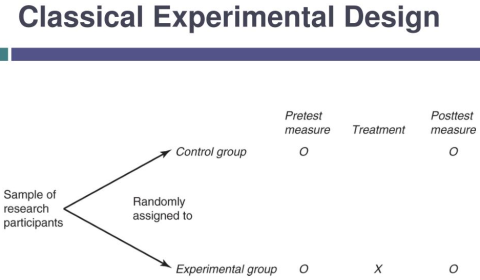
The issue here is that there never could be any evidence that the WHO would find acceptable, because such experiments would be unethical (ie the manipulation being performed in the experiment would never be allowed). The allegedly best scientific experiment (and experimental design is a subject that I professionally taught to university science students) is what is called a ‘double-blind treatment–control’ experiment (or sometimes a ‘randomised controlled trial’, or RCT), as shown in the next picture. In this, we take a randomly chosen group of people, and separate them into two groups: those who drink alcohol and those who do not. We then assign half of each group at random to the now-drink-alcohol (‘treatment’) group and half to the now-do-not-drink-alcohol (‘control’) group. Then we follow the resulting four groups of people through time, and see what medical and psychological benefits and problems arise.
It should be obvious to everyone that this procedure cannot be done ethically, and so no one has ever done it (even in the name of science!). Even worse, though, we should ideally do all of this in such a manner that the people involved do not know which of the four groups they are in, and nor do the people evaluating their behaviour (this is what ‘double blind’ means). Is this feasible? Of course not.
So, we will never have the best possible scientific evidence about the effects of alcohol on human health. The WHO is therefore correct in claiming that scientific evidence is lacking; but they are wrong in reaching any conclusions from this lack. This is certainly not how scientists proceed under these circumstances, anyway.
What the scientists do is the best that they ethically can. In this case, we follow large groups of drinkers and non-drinkers through time, and see how they get on – this is called an ‘observational’ study rather than a ‘manipulative’ one (as described above), of several types as listed in the next picture. In this type of study, health and behaviour experts measure all of the consistent differences they can between the people, to see what matches their patterns of drinking and non-drinking. There have been several summary publications in the medical literature reporting on these types of experiments.2 This is where all of the positive attitude towards consuming small amounts of alcohol came from, ten years ago.
So, all of the evidence regarding the effects of alcohol comes from experiments of the latter type. This type of rigorous analysis dates back to Raymond Pearl and his 1926 book Alcohol and Longevity (see Raymond Pearl on alcohol and longevity). If you want to read further, then the World of Fine Wine has several good posts (by Dr Erik Skovenborg), citing the pertinent literature.
Just as importantly for our purposes here, there is a difference between ‘hazard’ and ‘risk’, and the WHO does not seem to acknowledge this anywhere in their writings about the alleged effects of alcohol.
For example, for skin cancer there is a difference between the hazard [the sun] and the risk [getting skin cancer]. In this case, we try to control the hazard by addressing the risk. That is, we limit sun exposure to our bare skin as much as we can, and this keeps us as healthy as possible.
To take a behavioural example, getting into a car is unsafe from the first moment we do so. However:
- we give ourselves control of the car (eg steering, braking)
- we make using it as safe as we reasonably can (eg seatbelt, airbag)
- and then we get on with it (eg train people to drive safely).
Is there a hazard or a risk warning actually written on any car? No, because it is a societal issue, and we are all expected to know both the hazard and the risk. It seems to me that alcohol is much the same.
The WHO’s failure here tacitly assumes that alcohol is, in itself, the cause of all drinking problems, and that the amount of alcohol consumed determines the extent of any drinking problems (irrespective of the speed of drinking, the purpose of drinking, or the social environment involved). This is further discussed in Anti-alcohol industry 101: the neo-temperance movement.
Now, this does not mean that we should be complacent about potential health risks.3 After all, Wikipedia shows an increase in per capita deaths recently in several countries, and alcohol is sometimes involved. So, we should all be cognisant of the health risks of consuming alcohol. After all, people should not drink alcohol because they actually believe that it is always healthy for them! (See: Pour one out; and The truth about drinking a glass of wine every day, according to health experts.)
One important recent research publication about the risks is Alcohol consumption patterns and mortality among older adults with health-related or socioeconomic risk factors (2024 JAMA Network Open 7(8):e2424495). To quote from it:
‘While no associations were found for low- or moderate-risk drinking patterns vs occasional drinking among individuals without socioeconomic or health-related risk factors, low-risk drinking was associated with higher cancer mortality and moderate-risk drinking with higher all-cause and cancer mortality among those with health-related risk factors; low-risk and moderate-risk drinking patterns were associated with higher mortality from all causes and cancer among those with socioeconomic risk factors ... Wine preference (>80% of alcohol from wine) and drinking with meals showed small protective associations with mortality, especially from cancer, but only in drinkers with socioeconomic or health-related risk factors and was associated with attenuating the excess mortality associated with high-, moderate- and even low-risk drinking.’
The work done here looks good, to me, and the authors and funding look ‘clean’ from a conflict standpoint. Importantly, it addresses an apparent paradox, and comes to a fairly clear conclusion. This could turn out to be a key reference paper.
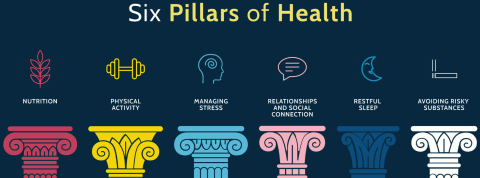
Equally importantly, we need to note that there is more to life than medicine (as shown in the picture above). That is, we need to weigh the relative benefits and risks of all of our health-related activities, together. This point was explicitly made in the editorial of The Lancet medical journal, replying to the WHO’s first publication of its new stance (Alcohol and health: all, none, or somewhere in-between?).
In particular, as Robert Joseph has noted: ‘we need to promote the unique, historic qualities of wine that make it such a great convivial product and such a delicious partner to food.’ That is, in the words of Erik Skovenborg, we need to note: Wine as part of a healthy lifestyle; and Drinking with friends: wine’s role as a social lubricant. If the wine label has to list the risks (as is being suggested for the new USA guidelines), should it also list the benefits? (eg Should alcoholic beverages have cancer warning labels?; or Is wine the ‘2024 cigarette’?)
Even at my advanced age, I still well-remember going down to the pub with my mates on Friday nights (at only 17 years of age!). I was one of the designated drivers, and therefore I drank lemon-squash, but the other guys certainly enjoyed their beers. These people were not just part of my official life (as a school student) but a part of my private life (as a part of society), and our interactions were highly valued in both roles (eg Couples who drink together live longer, study suggests; and Why social drinking is integral to a longer life). (See also: Rediscovering the fun in wine; and my own post: What are the current causes for optimism in the wine industry?)
In this sense, the new Drinks Insider’s Wine + Health series (by Felicity Carter) provides a podcast that is freely available. The first broadcast tackles anti-alcohol groups and drinking guidelines.
In this latter regard, we may well ask how so many temperance groups get to be advisors to the WHO (since 2018) (How neo-prohibitionists came to shape alcohol policy). Their presence (especially Movendi International, a heavily funded umbrella organisation for the neo-prohibition movement) is repeatedly noted in commentary on the current WHO attitude towards alcohol, and the bias that it generates seriously concerns me. This also leads to all sorts of accusations against researchers of alcohol effects (see The fight over moderate drinking: why studies on effects are unlikely to happen).
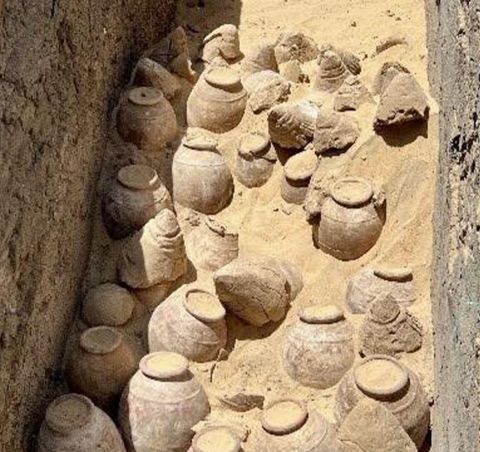
Let’s face it, we have been making wine for at least the past 6,000 years (Ancient winery found in Armenia), so it cannot be all bad for us, given how much our species has developed during that time. There are not many other creative things we have actual evidence of doing for that long. Surely, we would have dropped it, just like we have done for a lot of other things, if there was a major problem.4
However, even if the WHO does succeed with its current campaign (compare Gen Z continues shift away from alcohol with Why today’s reds are higher in alcohol), this does not mean that the wine industry must fade away. After all, we do have methods for reducing the alcohol content of wines, and we can even start to make alcohol-free wines worth tasting (Why alcohol-free wine is in the ascendant) – but that is a subject for another post (see also my previous post Fruit wine and alcohol-free wines really are also wines).
Footnotes
1 For example: Aaron E. Carroll, who teaches at the Indiana University School of Medicine, wrote, in an assessment of alcohol science, that: ‘15 desserts a day would be bad for you. This could lead to assertions that “there’s no safe amount of dessert.” But it doesn’t mean you should never, ever eat dessert.’
2 For example:
- Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. 2006. Archives of Internal Medicine 166(22):2437-2445.
- Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. 2011. BMJ 342:d671.
- Alcohol consumption over time and risk of death: a systematic review and meta-analysis. 2014. American Journal of Epidemiology 179(9):1049-1059.
3 For example, there is no doubt that heavy alcohol consumption damages your liver. The standard sort of disclaimer is something like this: ‘There are health risks associated with heavy alcohol consumption; and individuals with known health issues related to alcohol consumption, depression, or a family history of alcohol abuse, may not have any safe level of alcohol consumption.’
4 As Esther Mobley wrote: ‘I know that sugar, in high doses, is awful for me. But that doesn’t stop me from enjoying dessert after dinner a couple of times a week. There’s no question in my mind that the deliciousness of a piece of cake is worth whatever health trade-off I’ve made.’
Main image at top by Don Farrall via Getty Images.
Become a member to view this article and thousands more!
- 15,399 featured articles
- 274,619 wine reviews
- Maps from The World Atlas of Wine, 8th edition (RRP £50)
- The Oxford Companion to Wine, 5th edition (RRP £50)
- Members’ forum
- 15,399 featured articles
- 274,619 wine reviews
- Maps from The World Atlas of Wine, 8th edition (RRP £50)
- The Oxford Companion to Wine, 5th edition (RRP £50)
- Members’ forum
- Commercial use of our Tasting Notes